Hospitals and Healthcare Workers Struggle as COVID-19’s ‘Devastating’ Toll Continues
More Than 2 Million Dead Worldwide
Hospitals in Los Angeles are struggling. With the recent surge of Covid cases due to the holidays and related travel, hospitals are filling up, ICUs are full, and hospitals are running out of supplies.
“We are running out of gloves, oxygen tubes, ventilators. We run out of all types of equipment that you would never dream of a hospital running out of,” said ER doctor at Providence Cedars-Sinai Tarzana Medical Center Susan Urstein.
“It has been devastating over the last month,” Dr. Urstein said. Treating patients has been extremely challenging because doctors have to make decisions they are prepared for but never imagined: Who gets the ventilator?
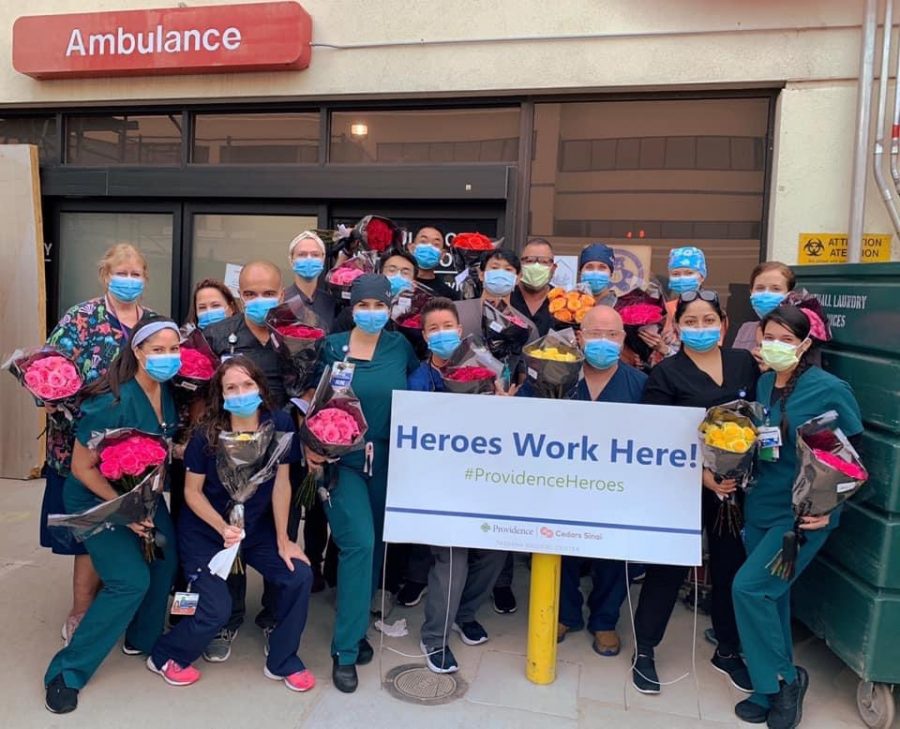
As soon as the first Covid-19 case broke out globally, ER doctors, surgeons, nurses, and all essential doctors put themselves on the line, risking their lives to help others. Health care workers valiantly report to their job sites daily to keep their communities safe.
Hospitals quickly adapted to the shocking situation by changing how they provided care: altering hours, repurposing their facilities, and taking every safety precaution needed to keep themselves, their families, and patients safe. On a day-to-day basis, healthcare workers are continuing to demonstrate their compassion and bravery despite the fears they may harbor.
In my interview with Dr. Urstein, she described the challenges she faces as a front line worker, the transformation of hospitals and patient care, and the accuracy of how the media is currently portraying Covid-19 in California.
According to Dr. Urstein, the first alteration was the ambulance traffic. Before COVID-19, it was relatively simple for ambulances to drop off patients; they would come in a specific door known as the “ambulance bay” and get checked in in front of the emergency room. However, that quickly changed when Covid-19 hit due to the uncertainty of knowing who had Covid and who didn’t. Patients are now kept outside until the paramedics connect with the doctors to figure out which room they should be put in.
The hospital has been converted into two sides, the “non-Covid” side and the “Covid side”.
“There’s an extra step, and there is a lot more waiting, which is actually very detrimental for the people in the community who might be calling 911,” Dr. Urstein said.
The next modification in patient triage involved walk-in patients, which took a 360-degree turn. “What has changed the most is that we try and do everything outside the hospital and get as many questions answered about their symptoms as we can to limit our exposure.” The triage for walk-ins has now moved to the parking lot, outside the hospital, except during the night shifts. The parking lot is tented and is now a triage and registration area. Doctors are given the patients’ symptoms, and from there, they cohort patients into a room.
When Covid-19 first broke out just over a year ago, two factors actually decreased the volume of patients coming into the ER, Dr. Urstein said. People were scared and didn’t come in when they probably should have, and more minor injuries were being dealt with at home, especially involving children, as they weren’t in school. In response to the decline in patients, the doctors at Providence Cedars-Sani Tarzana Medical Center were able to “cut two hours off each shift except overnight, and then we cut three complete shifts off the schedule each day,” she said.
After a few months, people started to become less scared and were willing to go into the hospital for injuries they should have come in for before. “It was horrible because people who were too scared to come to the ER were actually waiting at home when they had a heart attack two days ago.”
Even though the number of patients was decreasing for a while, when they did start coming back, patients’ “acuity” was much worse, which was extremely destructive, she said.
Healthcare workers have to take great precautions to keep themselves and their families safe. Dr. Urstein wears an N95 mask, a surgical mask, a surgical cap, and goggles for her entire shift. Along with that, she also brings a clean pair of scrubs to the hospital with her, so she can quickly change and go straight to her car at the end of her shift. When arriving home, she leaves her shoes out front and walks straight to the bathroom before doing anything. “Now, it’s a pain because I’m showering like a thousand times a day,” she said. Dr. Urstein’s precautions have not only prevented her from getting the virus but also kept her family safe.
“What we see now in Los Angeles is being accurately portrayed,” Dr. Urstein said about how the media is reporting on Covid-19 right now.
According to the New York Times, in Los Angeles County more than 5,000 people have died of Covid-19 in the last month, and one in every 10 people are getting the virus. On Jan. 23, there were 10,537 new cases and 269 new deaths, leading up to over 6,000 current hospitalizations in Los Angeles County.
As of Jan. 27, 2021, there have been over 100 million confirmed cases of Covid-19 globally and more than 2 million deaths, according to Johns Hopkins University Coronavirus Resource Center.
The site reports more than 25 million confirmed cases in the U.S. and 426,175 U.S.

My name is Payton Ozar, and I am a junior, new to de Toledo High School. I have always had a strong passion for writing, especially about current events,...




















Angela Neff • Feb 1, 2021 at 2:35 pm
Thank you for this truthful reporting on the painful reality of so many on the frontlines of Covid and those entering the hospitals as patients who do not make it out.
Ms. Neff